A silver lining during the COVID-19 pandemic has been the dramatic rise of technology as an enabler for service delivery. Virtual meeting tools and software have transformed sectors – for example, tele-medicine in health, virtual schools in education and digital marketplaces for agriculture. In this article, we talk about the promise of virtual platforms to deliver maternal and child health interventions, highlighting three innovations from our work across remote and rural villages of India.
The Antara
Foundation (TAF) strengthens health systems to improve maternal and child
health. Our programs train community health workers (CHWs), make data-sharing
more effective, build supervisory capacity and improve health facilities. The
lockdowns and safety measures imposed due to COVID-19 caused a slowdown in
several program activities due to travel restrictions, limitations on holding
large group meetings and the unavailability of health workers because of
additional COVID-response duties.
To address
this, our team redesigned elements of the program to deliver select activities
remotely, to supplement in-person trainings and maintain continuity of our
interventions.
1. Virtual
capacity building to improve essential MCHN knowledge
Our
capacity building work improves knowledge and skills of CHWs on essential
maternal, child health and nutrition themes. Detailed assessments are carried
out to identify knowledge gaps and inform the curriculum. The format involves a
mix of group trainings and on-site handholding for weaker staff. During the
pandemic, short virtual training packages were designed, with visually engaging
modules and interactive content such as handouts and quizzes. Feedback from the
CHWs was very encouraging.
Such
targeted virtual sessions are now a core part of our capacity building approach
to supplement in-person trainings. Their success stems from the following:
first, virtual sessions can be more personalized, targeted and interactive; second,
sessions can be scheduled with more flexibility to accommodate health workers’
busy schedules; third, they require fewer resources compared to classroom
trainings; and they have the potential to transform into self-sustaining peer
learning groups in the future.
2. Virtual nurse mentoring for government birthing nurses
TAF’s nurse
mentoring solution plugs critical knowledge and skill gaps in nurses who
conduct deliveries in government labor rooms. The comprehensive training
package covers 48 modules across seven key themes and is delivered through a
series of classroom sessions and live demonstrations.
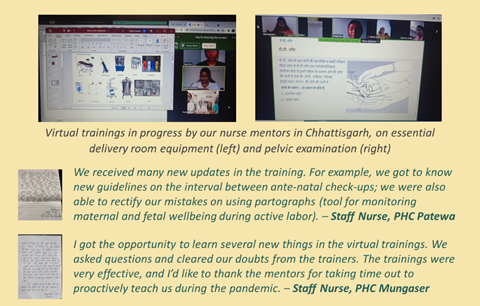
In our Chhattisgarh program, special virtual mentoring sessions were planned during COVID lockdowns to refresh concepts from previous trainings and discuss new modules. The format incorporated interactive case-based discussions, with pre and post online quizzes to increase engagement and ensure retention. The initiative proved immensely useful for the nurses to keep up to date and remain connected to their mentors and peers.
3.
Virtual AAA meetings
The AAA [Note 1] Platform is TAF’s flagship solution that brings the three community health
workers in each village on a collaborative data-sharing platform. The AAA
together create a detailed household level village map and mark critical
beneficiaries with different colored bindis. Each month, they meet to
pinpoint the highest-risk mothers and children, micro-plan service delivery,
and review each other’s work.
In
Chhindwara district, village maps have been created and installed in all ~900
villages of our focus blocks. Our team is now training the AAA to conduct
effective ‘AAA meetings’. During the lockdown, our team ran virtual AAA
meetings in select villages to help AAA identify high-risk beneficiaries,
develop follow-up plans, cross-check their data reporting, check availability
of medicines and supplies and recap essential knowledge.
The virtual
sessions involved collaborative discussion and data analysis. Several critical
action items were identified and promptly managed (e.g., anemic pregnant women
requiring urgent blood transfusion or iron sucrose, requirement for
antibiotics, iron and calcium tablets, vaccines).
We are enthusiastic about the early results from these targeted pilots. The willingness of health officials and CHWs to take to technology is encouraging. However, factors like device affordability, internet connectivity and basic IT skills are barriers still facing a large section of rural India. Until this ‘digital divide’ remains, scalability of purely virtual solutions will be a challenge. Meanwhile, we believe hybrid is the way to go, where technology supports and strengthens in-person grassroots health innovations.
Our
previous work in Rajasthan has shown the wonders technology can achieve. When
our ‘AAA Platform’ was taken up by the government for state-wide scale-up
across Rajasthan’s 46,000 villages, more than 125,000 CHWs were oriented
through video conferencing in a span of just a few weeks! Pilots of our ‘Integrated AAA App’ (mobile App for real-time data sharing
between CHWs) showed a significant increase in the identification of high-risk
mothers and children as compared to the offline process.
Note1: AAA
stands for ANM, ASHA and Anganwadi Worker – the three community workers who
deliver health and nutrition services in each village in India


Comments
Post a Comment